Is Obesity A Disease?
by Richard Weil, M.Ed., CDE
Founder and Director
Transformation Weight Control
The answer is an unequivocal YES.
This blog documents with images, captions, and commentary, the journey of obesity becoming recognized as a chronic disease by some of the most important medical agencies in the world. As they say, a picture’s worth a thousand words! And wouldn’t you rather look at pictures than read a thousand words! So, let’s get on with it. You’ll see images with a caption beneath it, with the expectation that you will become convinced that obesity is a disease, if you don’t already think so.
Here we go…
Kind of hard to challenge a dictionary definition. Sounds to me like it’s describing having obesity.
From Taber’s Medical Dictionary https://www.tabers.com/tabersonline/
–(diz-ēz′)– A condition marked by subjective complaints, a specific history, clinical signs and symptoms, and laboratory or radiographic findings.
I think we can all agree that subjective complaints, specific history, and certainly clinical signs and symptoms, can be applied to the clinical presentation of having obesity.
Laboratory findings related to obesity include, but are not limited to: low HDL (the ‘good cholesterol’), high LDL (the ‘bad’ cholesterol), high triglycerides, elevated fasting blood glucose (sugar) and glycohemoglobin A1C (the gold standard for diabetes testing), inflammatory biomarkers, thyroid health, liver function, and more. If you want to go the whole nine yards and spend a lot of money on expensive testing, you can measure levels of insulin, adiponectin, GLP, and appetite regulation hormones such as ghrelin, leptin, and CCK.
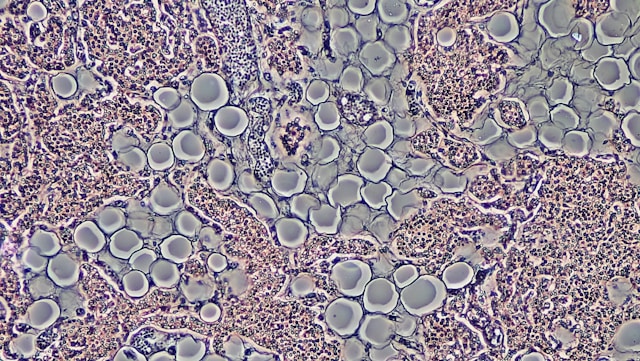
Radiographically, which is capturing images using MRI, CT scans, and PET scans, you could find disturbances in the brain such as inactive or low density dopamine receptors (i.e., down-regulated receptors), excessive activation of certain appetite centers in the brain, excessive subcutaneous body fat (fat directly below the skin all the way to the muscles), enlarged or high numbers of fat cells (adipocytes), and frequently excess visceral fat, the dangerous fat deep in the gut that surrounds and infiltrates vital organs such as the liver, which interferes with metabolic processes and can cause weight gain or resistance to weight loss.

This ground-breaking World Health Organization document published in 1997 clearly stated that obesity was a disease, specifically a ‘complex’, ‘incompletely understood’, ‘serious’ and ‘chronic’ disease which was part of a cluster of non-communicable diseases that required prevention and management strategies at both individual and societal level.
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for global public health. Headquartered in Geneva, Switzerland, it has six regional offices and 150 field offices worldwide. Their stated mission is to promote health, protect the world, and serve those who are vulnerable. Not exactly your neighborhood community board considering there are 198 countries and 8 billion people on the planet!
In 1998, the National Institutes of Health published Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults that stated, “Obesity is a complex multifactorial chronic disease.”
In early 2002, the Internal Revenue Service issued a ruling that expenses for obesity treatment would qualify as deductible medical expenses. Later in 2002, the Social Security Administration (SSA) published an evaluation of obesity stating that “Obesity is a complex, chronic disease characterized by excessive accumulation of body fat.”
Later in 2002, the Social Security Administration published an evaluation of obesity stating that “Obesity is a complex, chronic disease characterized by excessive accumulation of body fat.” From Kyle et al Endocrinol Metab Clin North America
In 2008, The Obesity Society, the major organization in the United States for the study of obesity, published a position stand on the evidence and arguments for obesity as a disease.
 In 2011, the NIH Obesity Task Force released the Strategic Plan for NIH Obesity Research. www.obesityresearch.nih.gov/
In 2011, the NIH Obesity Task Force released the Strategic Plan for NIH Obesity Research. www.obesityresearch.nih.gov/
In 2012, The American Association of Clinical Endocrinologists takes the position that obesity is a disease.


In June, 2013, the American Medical Association voted to recognize obesity as “a disease state with multiple pathophysiological aspects requiring a range of interventions to advance obesity treatment and prevention”. Furthermore, they stated that “recognizing obesity as a disease will help change the way the medical community tackles this complex issue.”
Of course this generated a lot of press.
The AMA is the largest association and lobbying group of all physicians and medical students in the United States since 1847. Membership was 271,660 in 2022. Their stated mission is “to promote the art and science of medicine and the betterment of public health.”
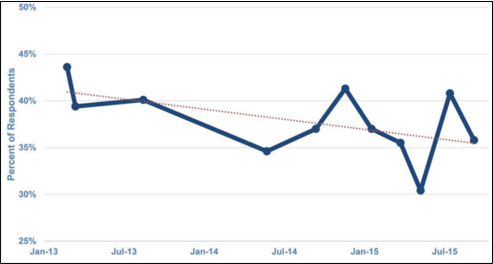
From Feb 2013 to March 2015 the proportion of the public that viewed obesity primarily as a “personal problem of bad choices” declined modestly from 44% to 36%. Adapted from Kyle et al., Presented at Obesity Week Conference 2015

This article by Kyle et al published in the journal Endocrinology and Metabolism Clinics of North America in 2016 is the finest I’ve ever read on the subject of obesity as a disease. It was very helpful for me when writing this blog. You can find it here: https://pmc.ncbi.nlm.nih.gov/articles/PMC4988332/pdf/nihms797211.pdf
 In May 2017, World Obesity published its position statement recognizing obesity as a disease.
In May 2017, World Obesity published its position statement recognizing obesity as a disease.
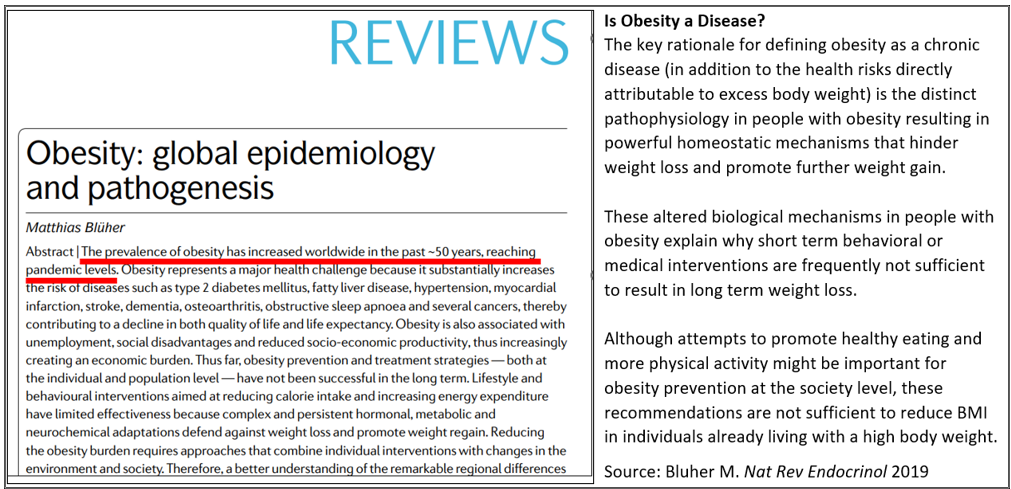 Source: Bluher M Nature Reviews | Endocrinology 2019
Source: Bluher M Nature Reviews | Endocrinology 2019
It’s worth repeating the excellent medical and persuasive explanation of why obesity is a disease, published in 2019 in the journal Nature Reviews | Endocrinology by M. Bluher
Dr. Bluher writes:
Is Obesity a Disease?
The key rationale for defining obesity as a chronic disease (in addition to the health risks directly attributable to excess body weight) is the distinct pathophysiology in people with obesity resulting in powerful homeostatic mechanisms that hinder weight loss and promote further weight gain.
These altered biological mechanisms in people with obesity explain why short term behavioral or medical interventions are frequently not sufficient to result in long term weight loss.
Although attempts to promote healthy eating and more physical activity might be important for obesity prevention at the society level, these recommendations are not sufficient to reduce BMI in individuals already living with a high body weight.
 The American Heart Association, in their 2021 Scientific Statement, is unambiguous about their stance on obesity as a disease.
The American Heart Association, in their 2021 Scientific Statement, is unambiguous about their stance on obesity as a disease.
On March 17, 2023, the IRS described the criteria for whether a weight-loss program can be deducted as a medical expense.
 In December 2023, the Obesity Medicine Agency does a very nice job of describing obesity as a disease.
In December 2023, the Obesity Medicine Agency does a very nice job of describing obesity as a disease.
 The American Society for Metabolic and Bariatric Surgery in 2024 pulls no punches when it comes to declaring obesity as a chronic disease and takes it further by describing the economic costs, as well as the negative effect on health, longevity, and psychological well-being. And then, rightly so, they describe the chronicity of obesity that requires life-long treatment and control, just like any other chronic disease you can think of. They get an A+ for this work.
The American Society for Metabolic and Bariatric Surgery in 2024 pulls no punches when it comes to declaring obesity as a chronic disease and takes it further by describing the economic costs, as well as the negative effect on health, longevity, and psychological well-being. And then, rightly so, they describe the chronicity of obesity that requires life-long treatment and control, just like any other chronic disease you can think of. They get an A+ for this work.
Some have argued that if obesity were a disease, it would be all over the world. Well, it is, and it’s spiraling upward. The graphs and numbers below tell the story⇓.
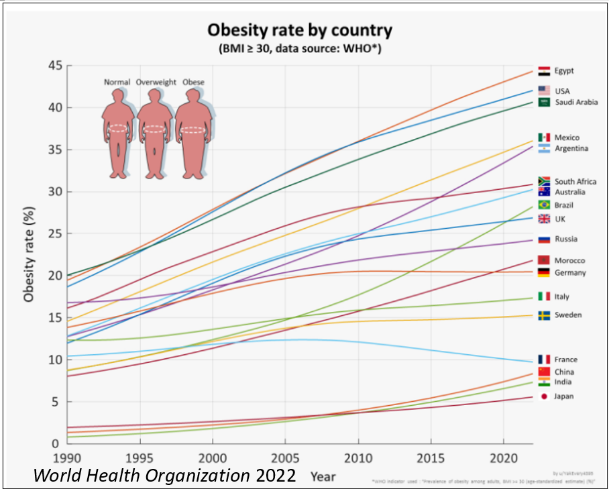
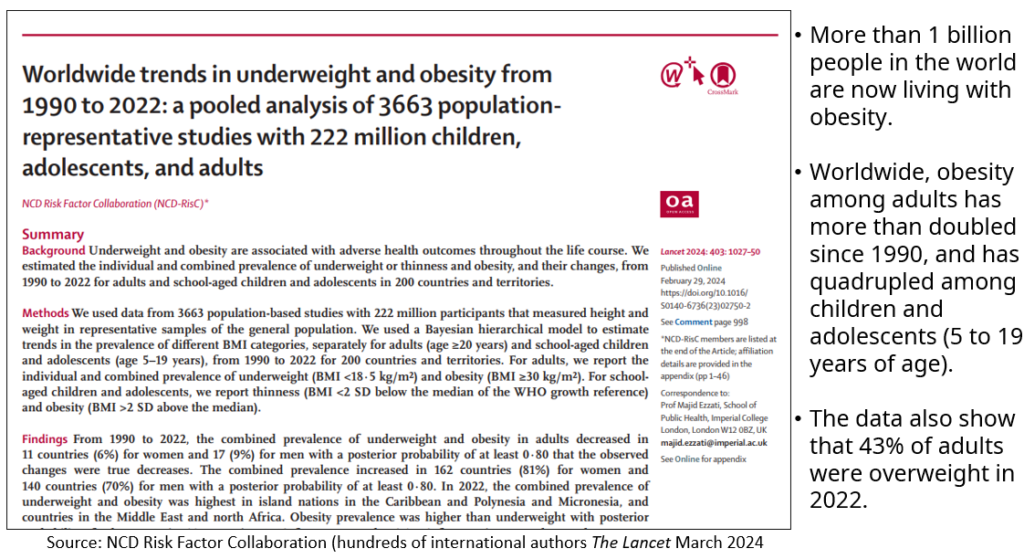
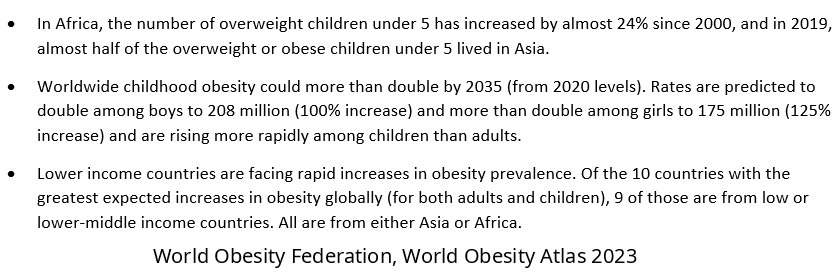
 Source: https://s3-eu-west-1.amazonaws.com/wof-files/World_Obesity_Atlas_2023_Report.pdf
Source: https://s3-eu-west-1.amazonaws.com/wof-files/World_Obesity_Atlas_2023_Report.pdf
The World Obesity Atlas Knows Something About Rising Rates of Obesity
The estimates for global levels of overweight and obesity suggest that over 4 billion people may be affected by 2035, compared with over 2.6 billion in 2020. This reflects an increase from 38% of the world’s population in 2020 to over 50% by 2035. The prevalence of obesity alone is anticipated to rise from 14% to 24% of the population over the same period, affecting nearly 2 billion adults, children and adolescents by 2035.
The rising prevalence of obesity is expected to be steepest among children and adolescents, rising from 10% to 20% of the world’s boys during the period 2020 to 2035, and rising from 8% to 18% of the world’s girls.
Two Main Arguments Against Labeling Obesity a Disease
In his article in Endocrinology and Metabolism Clinics of North America in 2016, Kyle presents two main arguments against declaring obesity a disease.
-
Argument #1: Concern about Weight Discrimination
Activists in the Fat Acceptance and Health at Every Size movements have consistently expressed opposition to this decision (calling obesity a disease), anticipating that its primary effect would be to promote size and weight discrimination. In another NIB essay, Jennifer Hansen expressed this view: “Classifying obesity as a disease provides more ammunition for the ‘war on obesity.’ From a fat person’s perspective, the ‘war on obesity’ is a war on fat people.”
My Comment
Jennifer Hansen seems to be unaware of how strong, insidious, and ubiquitous the bias and discrimination against people with obesity already is. More ammunition for the ‘war on ‘obesity’ if we call obesity what it is, a disease, is what she thinks? How much worse could it get? And to use the word ‘fat’ to describe you, depending on who you are and how you handle this sort of judgement, can be even more pejorative, stigmatizing, and damaging than being called ‘obese’, which we no longer do because it negatively labels you, just like saying someone is diabetic. This type of labeling creates a clear distinction between ‘us’ and ‘you’, perpetuating the isolation, amongst many other negative psychological consequences. No, we now say, this person ‘has’ diabetes, or this person ‘has’ obesity. Because diabetes or obesity does not define who you are as a person. At TWC, we refer to the phenomenon of defining yourself by your disease as ‘false equivalence’.
But these thoughts of mine are not even the major point I want to make. The point is that for the 44 years that I’ve been treating people with obesity, I’ve always taught the biology and the psychology of this chronic disease, and it doesn’t devastate anyone. Just the opposite. It empowers you, improves your self-esteem, your self-confidence, and your self-efficacy. It decreases depression, builds your resilience, and takes the pressure off so that you don’t beat yourself up thinking having obesity is your fault and that for every failure you deserve to be punished. IT IS NOT YOUR FAULT.
Teaching the science of obesity, and proving that it is truly a disease, helps you understand what’s really going on inside your body, and proves definitively that it is not your fault. Teaching that obesity is a chronic disease is the sensitive, sensible, effective, and compassionate thing to do. It’s probably not polite to say so, but Ms. Hansen, and anyone who agrees with her viewpoint, do not know what they are talking about.
-
Argument #2: Concern about Personal Responsibility
Michael Tanner captured this perspective in the National Review: “At first glance, it’s a minor story, hardly worth mentioning, but in reality, the AMA’s move is a symptom of a disease that is seriously troubling our society: the abdication of personal responsibility and an invitation to government meddling.”
My Comment
To claim that calling obesity a disease will cause you to abdicate responsibility for your disease suggests that the disease is your fault. IT IS NOT. Obesity is a multi-factorial biological and psychological disease caused by genetic mutations, hormonal imbalances, appetite dysregulation, aberrant neurobiology, especially in the reward pathway of the brain, but also dopamine receptors that are either reduced in numbers, reduced in density, or are otherwise less active than they should be (a sure sign of addiction to food, another story altogether), metabolic disturbances including, but not limited to, insulin resistance and poor glucose regulation, body image disturbances, societal bias and discrimination, a toxic food environment, and dozens of other factors. I don’t know a soul on this planet who woke up one day and thought how cool it would be to have obesity and addiction to food.
What it tells me about Michael Tanner is that he has no sense of what it is to live with obesity, nor does he understand anything about the biology of the disease. He’s clearly not a clinician and obviously has never worked with individuals who live with this disease to observe first-hand the challenges, the pain, the suffering, the isolation, the failures, the low self-esteem, the self-loathing, the depression, the lack of self-compassion, the shame, and so much more, that individuals with obesity live with every day.
Instead, it speaks to his bias against you if you have obesity. He suggests that you are irresponsible, and that you should take responsibility for your actions and simply eat less and exercise more. No one would ever say anything like this about individuals with other chronic diseases such as diabetes or high blood pressure. Only obesity. His comment about abdication of responsibility if obesity is considered a disease is offensive. And I have no idea what he means by government meddling. Hundreds of chronic diseases exist, how is the government meddling?
The Future
In the future, perhaps identifying obesity as a disease will help pass legislation to help you with the problems and challenges of having obesity. For instance, Medicare has never been allowed to pay for weight loss medication, but in a stunning reversal, they are now paying for the weight loss medication Wegovy if you have pre-existing cardiovascular disease. And maybe labeling obesity for what it is may create a protected class of people who can no longer be freely and legally discriminated against in the work place, or anywhere else, and if you are, you have a potential lawsuit that you can possibly win in court.
I could go on and on about this topic, but I think you already have a good idea where I stand on these issues. I hope that at some point we all come to our senses, stop the discrimination, the shaming, the blaming, and accept that obesity truly is a chronic disease, and the only approach that makes sense is one of compassion and support.
Join us at TWC. We’ll show you the way and you’ll get all the help you need.
If you’d like to read more about topics related to this one, visit our blog page by clicking HERE, and on the left border, scroll down to the search box and type in ‘addiction’ or ‘bias’.
© Richard Weil, M.Ed., CDE, 2025, All Rights Reserved