by Richard Weil, M.Ed., CDE
Founder and Director
Transformation Weight Control
Inflammation is one of those words that’s thrown around a lot when it comes to disease, yet I suspect many people don’t know what it really is. My plan with this blog is to enlighten you, and describe why control of body weight is so important in the role of managing inflammation.
What It Is
Inflammation is a critical response by the immune system for the body to heal from infection, disease, and injury. It plays a vital role in the healing process. However, there’s an upside and a downside to inflammation, characterized by two types of inflammation.
The Two Types of Inflammation Are:
Acute and chronic…
Acute inflammation is a short-term process occurring in response to tissue injuries such as a splinter, burn, or laceration, and can be resolved within a few hours or days. This is the redness, warmth, swelling, and pain around tissues and joints that occur in response to an injury. When the body is injured, your immune system releases white blood cells to surround and protect the area. In acute inflammation, your body will return to its previous state as soon as your injury has been treated.
Chronic inflammation is, as the name suggests, a long-lasting form of inflammation. It can go on for months or even years. With chronic inflammation, the immune system continuously releases white blood cells because it thinks it’s constantly injured. Its effect does not end when the injury or illness is healed. Chronic inflammation is associated with many diseases, including chronic obstructive pulmonary disease, colon and breast cancer, fibromyalgia, chronic fatigue syndrome, allergies, inflammatory bowel disease (Crohn’s disease and ulcerative colitis), depression and anxiety, insulin resistance, auto immune diseases (such as lupus, rheumatoid arthritis, gout, and psoriasis), nephritis (inflammation of your kidneys which can cause high blood pressure or even kidney failure), diabetes, cardiovascular disease, obesity and impaired fat cells (more about the role of losing weight shortly), and asthma. Inflammation can also affect the neurological system, which can be associated with depression and anxiety, dementia, autism, ADHD, memory loss, and Alzheimer’s and Parkinson’s disease.
Causes of Chronic Inflammation
There are many causes of chronic inflammation. Having obesity, stress and anxiety, smoking, poor sleep habits, a diet that includes trans and saturated fats, highly processed foods, added sugar and artificial sweeteners, high intake of alcohol, exposure to toxins in the environment such as pollution and some chemicals, an unhealthy gut microbiome, inactivity, and older age are all associated with chronic inflammation.
Tell-tale Signs of Chronic Inflammation
There are many symptoms associated with chronic inflammation. Some of the common symptoms include joint pain, swelling, and stiffness anywhere on the body, chronic fatigue or insomnia, and frequent infections. Skin rashes, depression or anxiety, mouth sores, and gastrointestinal problems such as diarrhea, constipation, bloating, or abdominal pain, are also possible. Your primary care provider is a good place to start if you have any of these symptoms. He or she will take a careful history, and blood tests, to make the diagnosis, and then, if necessary, refer you to one of several kinds of specialists. Common biomarkers of chronic inflammation are levels of red and white blood cell count, hemoglobin count, C-reactive protein (CRP – a type of protein produced by the liver in response to inflammation), and sedimentation rate (when red blood cells sink faster in a test tube than normally expected). There are many treatment options depending on the condition of your inflammation.
Why a Blog About Inflammation in a Weight Control Program?
The title of this article, published in 2018 in the journal Clinical Nutrition ESPEN, says it all. The author reviewed and summarized 76 studies about the effect of weight loss on chronic inflammation. The title of the article is also the author’s conclusion.
Why Does Losing Weight Reduce Chronic Inflammation?
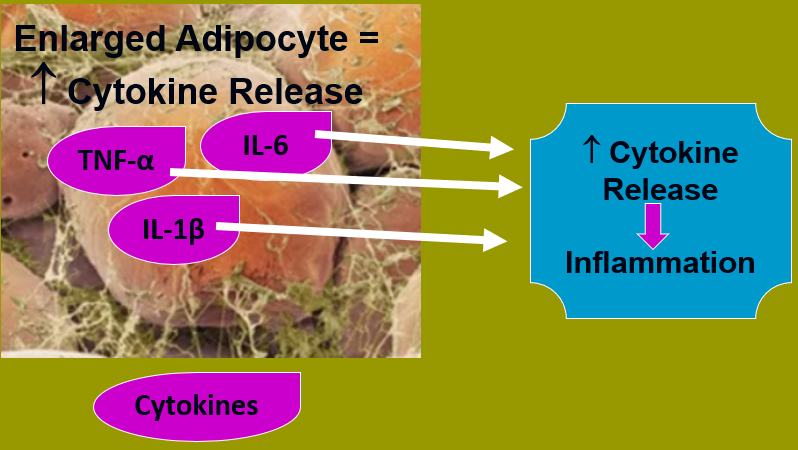
Cytokines
Cytokines and adipokines, a type of cytokine, are proteins, some of which are released from fat cells (adipocytes and adipose tissue), and are an important part of the immune system. TNF-alpha, IL-6, and IL-1β, are examples of cytokines. These cytokines play an important role in the immune system to reduce inflammation and signal other immune system cells to do their job and also reduce acute and chronic inflammation. But when you have excess body fat, fat cells get large and secrete too many cytokines, which, instead of reducing inflammation the way cytokines and adipokines are supposed to, will c contribute to chronic inflammation. Losing weight reduces the size of fat cells, which in turn will lower the over-production of cytokines and adipokines, and thus lower inflammation levels.
Visceral fat
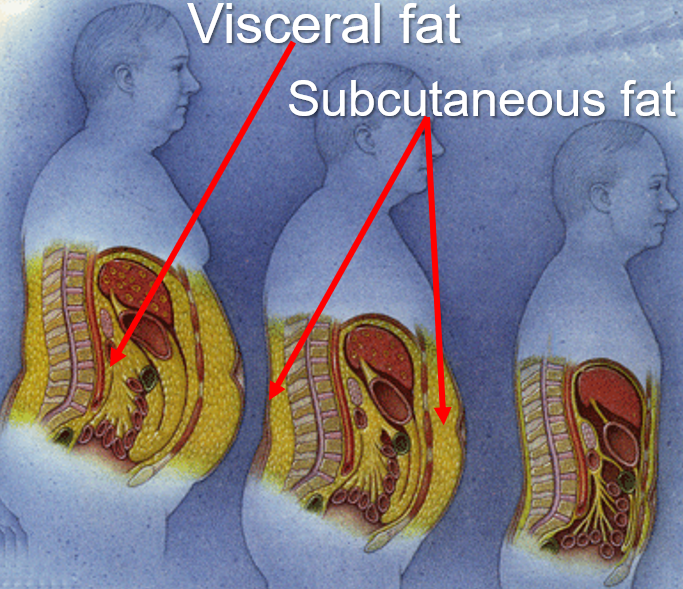
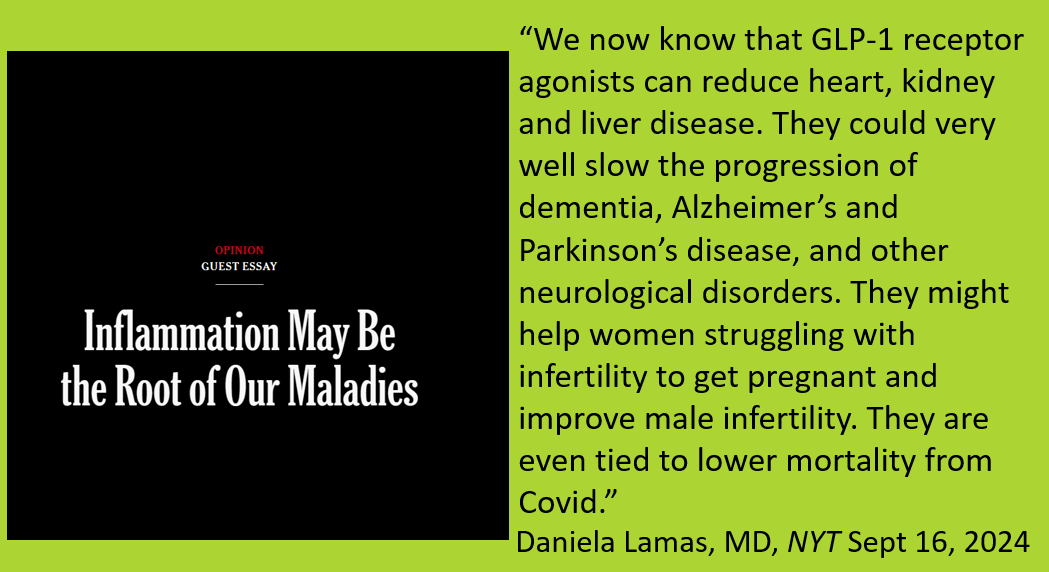
- Visceral fat produces excess inflammatory cytokines. Visceral fat – as opposed to subcutaneous fat just below our skin, see the graphic below – is the most dangerous kind of fat, much more so than subcutaneous fat, and is found deep in our gut. It surrounds and infiltrates internal organs such as the liver, kidneys, pancreas, intestines, and the adrenal glands, causing dysfunction in these organs which can lead to lead to diseases such as diabetes, fatty liver disease, kidney disease and other metabolic and cardiovascular disorders. The adrenal glands, which produce the stress-hormone cortisol, when inflamed, will negatively influence hormone regulation, the stress response, and store fat in your abdomen. None of this is obviously healthy for our bodies. The good news is that losing weight decreases the size of fat tissue, which will lower over-production of cytokines and in turn reduce chronic inflammation. The anti-obesity medication GLP-1 receptor agonist has a similar effect, working most of its magic by reducing inflammation.
- The simplest and safest method at home to estimate how much visceral fat you have and predict metabolic disease, instead of an expensive CT scan which uses radiation, is to measure your abdominal circumference across the belly button, typically the widest part of the belly (shown below). Abdominal fat is called a “proxy” for visceral fat, it estimates it; men should have an abdominal circumference of 40 inches or less, and 35 inches or less for women.

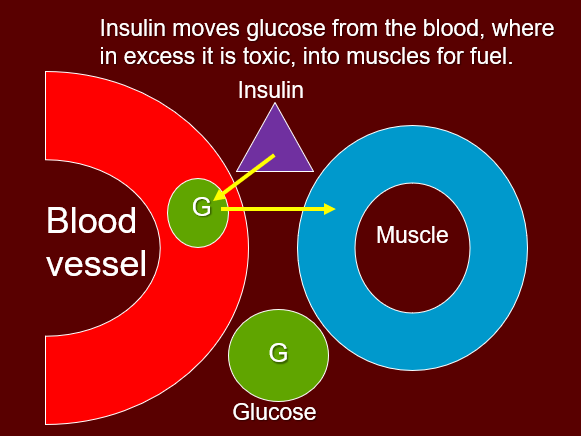
- Losing weight improves insulin sensitivity. Insulin is a hormone released by the pancreas when you eat that helps move blood sugar out of the blood where it is toxic, into muscle and other cells. High insulin resistance causes insulin to dysfunction, lading sugar in the blood to accumulate, which negatively affects nerves, major large blood vessels, and smaller capillaries in the eyes, causing an eye condition known as diabetic retinopathy which will lead to visual disturbance and possible blindness. Reducing the risk of these negative outcomes by improving insulin resistance will reduce or prevent the incidence of type 2 diabetes, which is associated with chronic inflammation.
- Certain bacteria in the gut are beneficial for the gut microbiome. The microbiome contains microorganisms or microbes such as bacteria, viruses, and fungi. When the microbiome is dysfunctional, it can play a role in inflammation and having obesity. Weight loss improves the microbiome. There is a great deal of research attempting to learn more about the role of the microbiome.
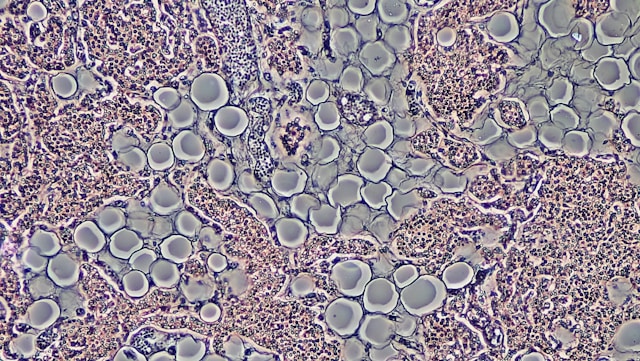
- Macrophages are a type of white blood cell that plays a critical role in the immune system. When individuals have obesity, there is an accumulation of immune cells, particularly macrophages, in adipose tissue. When the macrophages become activated, they release additional inflammatory cytokines, exacerbating the inflammatory cycle.
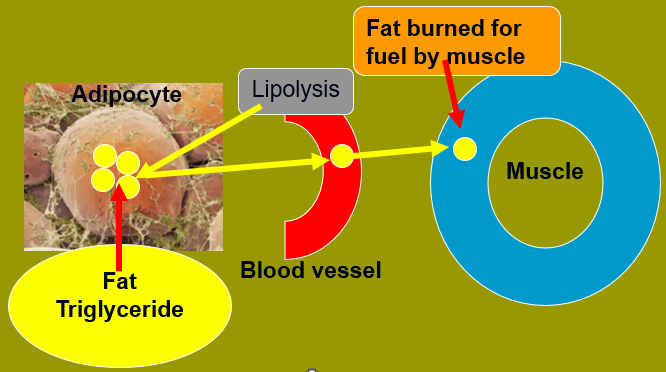
- Lipolysis is a biochemical process that breaks down triglycerides (fat) stored in the adipose tissue (adipocyte). Then, the fat moves into the blood stream, where it is transported to muscle to be burned for fuel. Adipocytes in an inflamed state will increase lipolysis and release excess fat (free fatty acids) into the bloodstream, contributing to chronic inflammation as well as metabolic disturbances.
- The endoplasmic reticulum (ER) is a structure located in cells that is necessary for cell survival and healthy cell performance. Having obesity will cause ER stress in adipocytes, which triggers chronic inflammatory responses and leads to metabolic disorders such as diabetes, high blood pressure, cardiovascular disease, and stroke.
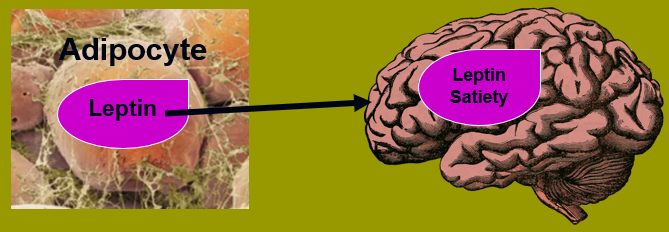
- Inflammation impairs the production of a key hormone called leptin, which works in the brain as a messenger to regulate metabolism and control appetite. Lower levels slow metabolism and make you feel hungry, further impeding any efforts to control weights.
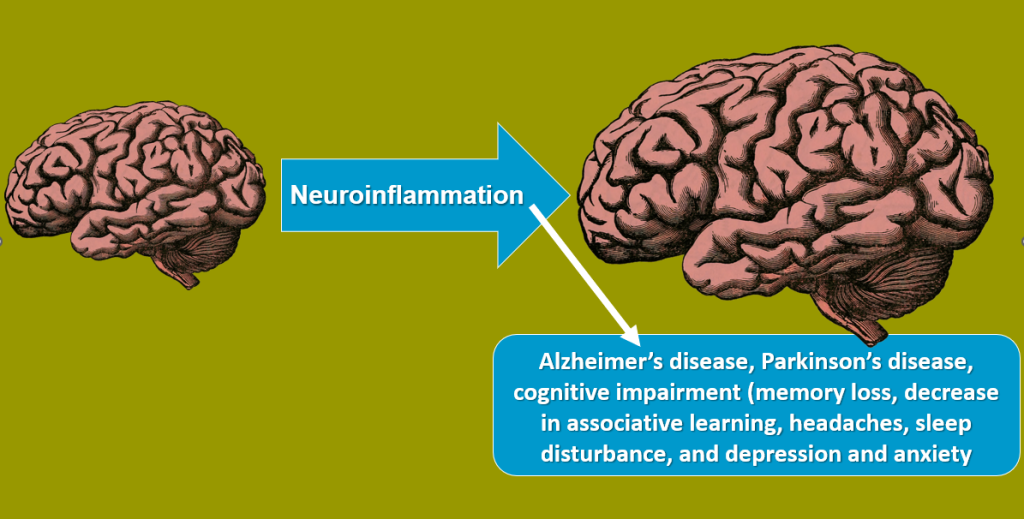
- Neuroinflammation (inflammation in the brain) is associated with Alzheimer’s disease, Parkinson’s disease, cognitive impairment (memory loss, decrease in associative learning, headaches, sleep disturbance, and depression and anxiety).
- And a Final Shout Out to GLP-1 Receptor Agonist Anti-Obesity Medications and Chronic Inflammation
IN SUMMARY
Chronic inflammation leads to organ dysfunction, metabolic disfunction, and more, creating disease and poor physical and mental health as described above. Overall, losing weight plays a significant role in reducing chronic inflammation.
© 2025 Richard Weil, M.Ed., CDE All Rights Reserved