by Richard Weil, M.Ed., CDE
Founder and Director
Transformation Weight Control
I like to show the following slide when discussing side effects of GLP-1 receptor agonists. It shows the potential side effects of 12 of the most common prescription and over-the-counter medications in the U.S. The point is not that you should be able to read all the side-effects, but rather impress upon you that all medications have potential side effects, and many have lots of them!
The GLP-1 receptor agonists approved for weight loss include: Zepbound (tirzepatide), Saxenda (liraglutide), and Wegovy (semaglutide). All of them have similar side effects, the most common being nausea, diarrhea, vomiting, and constipation. More serious side effects include pancreatitis, changes in vision, low blood sugar (hypoglycemia), allergic reactions, acute kidney injury, and severe stomach problems. I’ll discuss the most common side effects in this blog.
The most frequently reported side effects, by percent, for GLP-1s, was reported by Liu and colleagues in the journal Frontiers in Endocrinology in December 2022. They found that for FDA approved GLP-1s for weight loss, liraglutide (Saxenda) and semaglutide (Wegovy), the percent of side effects reported was as follows:
-
Nausea: 42.2%
-
Diarrhea: 21.9%
-
Vomiting: also 21.9%
-
Constipation: 8.4%
They report that although the incidence of side effects were similar among medications, semaglutide had the greatest risk of nausea, diarrhea, and vomiting, whereas liraglutide had the greatest risk of upper abdominal pain. This may be helpful information if you are having side effects and want to switch from one weight-loss approved GLP-1 to another.
For tirzepatide (Zepbound) Jastreboff and colleagues reported in the New England Journal of Medicine in 2022 that at maximal doses, the percent of individuals reporting side effects were as follows:
-
Nausea 31.0%
-
Diarrhea 23.0%
-
Vomiting 12.2%
-
Constipation 11.7%
Bettge and colleagues conducted a study published in Diabetes, Obesity, and Metabolism in 2017 that showed that individuals who were taking metformin while taking a GLP-1 were more likely to have side effects, especially nausea and vomiting.
Here are some suggestions for managing the common side effects. CONSULT YOUR PHYSICIAN IF ANY OF THESE CONDITIONS PERSIST
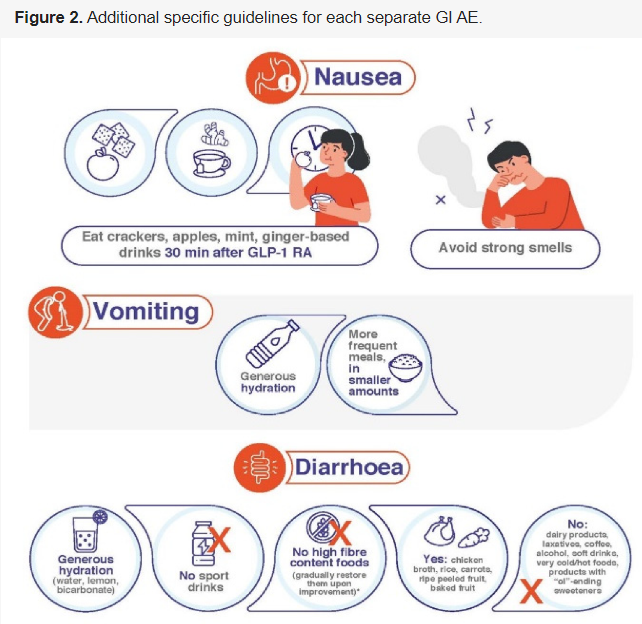
Nausea (usually the most common side effect – up to 50% of all patients may experience nausea)
-
One of the best ways to avoid nausea is to stay hydrated. Because GLP-1s reduce hunger and appetite, resulting in you consuming less food and fluids, it’s important that you stay hydrated (eight 8-ounce glasses of water a day).
-
Your doctor may recommend lowering the dose of your GLP-1 medication, or prescribe an anti-nausea medication.
-
According to Novo Nordisk, the maker of Saxenda and Wegovy, they recommend eating bland, low-fat foods, such as crackers, toast and rice; or foods that contain water, such as soups and gelatin, and skip sweet, sugary foods and drinks, and avoid or limit alcohol intake.
-
Don’t eat or cook strong-smelling food.
-
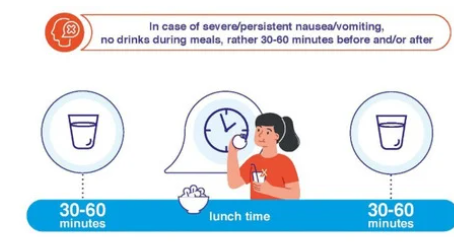
Don’t eat too quickly and don’t have a large drink with meals.
-
Don’t lie down soon after eating. Wait at least 2-3 hours after eating a meal to lie down. This will reduce pressure on your abdomen.
-
Avoid high-processed foods, and sometimes limiting red meat will help.
-
Medications that may be effective against nausea and diarrhea are antiemetic drugs, although evidence is limited: Benadryl, Bonine, Phenergan, Dramamine, Gravol. Speak with your doctor before taking any of these.
-
Eat smaller meals.
-
Eat slowly and stop when satisfied. Pay attention to your fullness.
MEDICATIONS
FOR ALL MEDICATIONS, PRESCRIPTION OR OVER-THE-COUNTER, ALWAYS SPEAK WITH YOUR DOCTOR FIRST!
I. Medications for Nausea and Vomiting (OTC: Over-the-Counter)
- Meclizine (Bonine) – OTC at low doses (25mg), prescription for higher doses (50 mg or more)
- Dimenhydrinate (Dramamine) – OTC
- Nauzene-OTC
- Pepto-Bismol-OTC
- Dramanine-OTC
- Emetrol – OTC
- Ondansetron (Zofran) by prescription (check with your doctor, it can cause constipation, a GLP-1 side effect)
- Metoclopramide (Reglan for GERD) by prescription (check with your doctor, it is used to treat gastroparesis which means it increases gastric emptying. GLP-1s work by delaying gastric emptying.)
- Ginger supplements or ginger tea can sometimes alleviate nausea.
- Antacids: Famotidine or Omeprazole can help with acid reflux or heartburn (OTC or prescription depending on dose).
II. Diarrhea (the second most commonly reported side effect)
-
-
Avoid greasy or spicy foods and limit caffeine and alcohol.
-
Avoid high-fat foods, sugary beverages, and full-fat dairy products such as milk, cheese, yogurt, and ice cream.
-
Avoid beverages that contain sorbitol, mannitol, and xylitol, or any other artificial sweetener
- No dairy or any citrus fruit, (no milk or anything with dairy). Nothing with high fructose corn syrup.
-
-
- Stay hydrated with drinks such as water, fruit juices (unless they cause nausea), and broth
-
-
Eat smaller, more frequent meals, instead of larger meals.
- A bland diet: bananas, rice, applesauce, toast (white bread only). Vegetable broth, oatmeal, and if it doesn’t make you feel ill, you can try bland cooked chicken in small amounts (but no pork, veal, red meat), cottage cheese, boiled or baked potatoes (no butter), crackers, tea (decaf, no caffeine in anything), and peanut butter.
-
-
- VERY LOW fiber foods (no high fiber vegetables: e.g., beans, broccoli, kale, corn prunes, peas).
-
- If you are hungry eat smaller meals throughout the day rather than 3 large meals. Eat slowly and pay attention to how your gut feels.
-
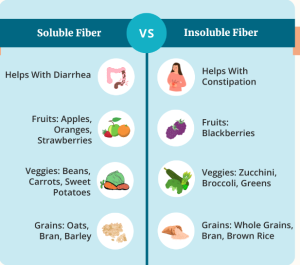
You may be consuming too much fiber. If that’s the case, eat foods that have less fiber. Here are authoritative and accurate fiber resources:
Medications for Diarrhea:
- Imodium, Pepto-Bismol, Kaopectate, Maalox, all over the counter.
- Lomotil, but ask your doctor first.
- Drink plenty of fluids to avoid dehydration (water or sports drinks, you can dilute the sports drink with water)
- IT’S VERY IMPORTANT to hydrate at least 6-8 ounces after each loose bowel movement.
- Proton pump inhibitors (PPIs) help relieve symptoms of GERD and stomach ulcers.
- Read this: https://my.clevelandclinic.org/health/articles/proton-pump-inhibitors
- Omeprazole (Prilosec) – OTC
- Nexium (can be OTC in small doses, otherwise by prescription))
- Prevacid – OTC
- Gradual titration: Starting with a lower dose and gradually increasing can help the body adjust to the medication.
III. Vomiting (the third most commonly reported side effect)
-
Stay hydrated. Eight 8-ounce glasses of water a day
-
Eat more frequent meals in smaller amounts.
-
Don’t eat or cook strong-smelling food.
-
Avoid large drinks with meals.
-
Eat slowly and stop when satisfied. Pay attention to your fullness.
Medications for Vomiting (see the medications for nausea in medications for nausea and vomiting above)
IV. Constipation (the fourth most commonly reported side effect)
-
Drink lots of fluids, eight, 8-ounces glasses of water a day.
-
Eat more foods with a high fiber content. See # 8 under Diarrhea for links to learn more about fiber. Some simple tips are:
-
Choose foods that have at least 4 grams of dietary fiber per serving.
-
Add more beans to your diet.
-
Eat more fresh fruits and vegetables, especially with the skins on.
-
Look for foods with 100% whole wheat, rye, oats, or bran.
-
Consume prunes and prune juice.
-
Ask your doctor about over-the-counter laxatives.
-
-
Talk with your doctor about fiber supplements, or medications/treatments for constipations such as stool softeners. It may be that you are not as hungry as you used to be and eat less because of the medication, so a fiber supplement may be indicated. Again, speak with your doctor abut this.
-
Exercise helps move stool through the digestive tract (increased gastric motility).
Medications and other Remedies for Constipation:
- Colace-OTC stool softener
- Dulcolax laxative – OTC
- Senna – OTC
- Magnesium can sometimes be helpful
- Lactulose (prescription)
- Linaclotide (prescription)
- Lubiprostone (prescription)
Dietary modifications for constipation:
- Eating smaller, more frequent meals and avoiding high-fat
foods can help minimize gastrointestinal discomfort. - Soluble and insoluble fiber can help with constipation, but
insoluble fiber is generally more effective. - Fiber supplements:
- Metamucil – OTC
- MiraLax – OTC
- Milk of Magnesia – OTC
- me – OTC
- Hydration: 64 ounces per day.
- Probiotics:
- Align pro-biotic https://www.alignprobiotics.com/
- Acidophilus (most well-known beneficial bacteria)
- Possible side effects from acidophilus include:
- Constipation
- Gas
- Bloating
- Increased thirst
- Sources of Probiotics:
- Sauerkraut
- Yogurt
- Kefir
- Kimchi
- Tempeh
- Miso
- Sourdough
- Olives
- Cheese
- Kombucha
Toilet posture for constipation: Raise your feet 6-9 inches off the floor when you are sitting on the toilet. Use a step stool or a thick book(s). This will position your body to reduce straining.
A Few Other Points to Consider
-
Some of the side effects seem dose-dependent, that is, the higher the dose, the more likely it is that you will experience side effects. This is why your doctor may lower your dose if you have side effects that are difficult to tolerate.
-
Most common side effects are usually mild to moderate and tend to resolve on their own. If they don’t, then you should speak with your doctor.
-
In some cases, no GLP-1 will be tolerable. If that happens, it may be worth considering some of the other medications approved for weight loss that are not GLP-1s. Those are Qsymia, Contrave, Plenity, Phentermine, Xenical and alli over-the-counter (alli does not require a prescription).
Thyroid Cancer
Much has been written and spoken about the potential risk for thyroid cancer in individuals taking GLP-1s. These comments are based primarily on research in rats who were administered GLP-1s and developed thyroid cancer. Studies in rodents don’t always translate to humans. The first GLP-1 receptor agonist, exenatide, was developed in 2005 and safely prescribed ever since. I have been a Certified Diabetes Educator since 1986 and in all those years can’t recall a case of thyroid cancer from taking a GLP-1. That doesn’t mean it hasn’t happened, I have just not observed it. More important than my observation is the following:
-
In comments by Thompson and Sturmer published in the journal Diabetes Care in 2023, about a study of GLP-1s and the risk of thyroid cancer conducted by Bezin et al which was published in the same journal issue, Thompson and Sturmer conclude that “Thyroid cancer is a rare outcome, however, and the potential increase in absolute risk is very small. Clinicians and patients need to always balance benefit and harm of treatments in light of their alternatives. In a population without specific risk factors for thyroid cancer, the benefits of GLP-1 RAs will largely outweigh the harm.”
-
The European Medicines Agency in October 2023 announced that they did not find a causal link between GLP-1s and thyroid cancer after a months-long review.
-
Lisco and colleagues published a review of the risks of GLP-1s and thyroid cancer in the journal Endocrine Connections in 2023, and although they describe evidence for a risk of thyroid cancer, they conclude: “It is reasonable to continue prescribing GLP-1RAs due to the evidence of more relevant and well-recognized antihyperglycemic, cardiovascular, and renal benefits, with the management staying within current recommendations.”
If you are considering taking a GLP-1 but are concerned about the risk of thyroid cancer, you should discuss it with your doctor. He or she can run tests and there is also genetics counseling available to determine your risk.
Some Final Tips
In a study of GLP-1 side effects, Gorgojo-Martinez and colleagues published the following infographics in the Journal of Clinical Medicine in 2023 about how to manage GLP-1 side effects. Here are those infographics.

© 2025 Richard Weil, M.Ed., CDE, All Rights Reserved